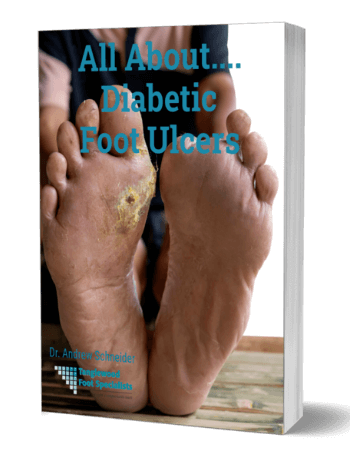
Unfortunately, about 6.5% of diabetics will develop an ulcer in their lifetime, meaning it is a common and dangerous complication of diabetes. In fact, diabetic foot ulcers are actually more deadly than most cancers. (Only lung and pancreatic cancer have a worse five-year survival rate.) But why are ulcers so dangerous, and how can we heal them to prevent serious complications? Here's what you need to know.
Unfortunately, about 6.5% of diabetics will develop an ulcer in their lifetime, meaning it is a common and dangerous complication of diabetes. In fact, diabetic foot ulcers are actually more deadly than most cancers. (Only lung and pancreatic cancer have a worse five-year survival rate.) But why are ulcers so dangerous, and how can we heal them to prevent serious complications? Here's what you need to know.
Why Do Ulcers Form?
Think of these ulcers as open wounds that typically develop on pressure points across your feet. And that's not a coincidence: an ulcer forms because of increased pressure beneath the foot, combined with the fact that diabetes can damage your nerves, compromising sensation in your feet and making it harder for you to notice damage to your feet. Over time, you can have excessive pressure on the foot, leading to a breakdown of the skin. Then, because diabetes also affects your circulation, reducing blood flow to your feet, even small injuries can take longer to heal, allowing an open ulcer to form.
Preventing Ulcer Formation
First and foremost, we must manage your diabetes to help prevent ulcers from forming. Think about this scary statistic: every point your A1C rises above normal results in a 10-fold reduction in your body's healing abilities. That means that if your A1C is just one point too high, your body's healing ability is reduced by 1000%. As such, maintaining your blood sugar levels isn't just about preventing complications; it's about giving your body its best chance to heal if problems do develop.
Another way to prevent ulcers is by performing daily foot checks. Make this step an automatic part of your routine, like brushing your teeth. You need good lighting and a mirror to check the bottom of your feet. During the exam, look for more than just obvious cuts or sores, or even small areas of redness or spots that feel warm. You must also look for :
- Moisture or skin changes between your toes
- Signs of wear and tear on your heels or the balls of your feet, which bear the most pressure when you walk
If you notice any differences in the appearance of your feet during this daily exam, seeking immediate attention is critical. This can help us detect an ulcer in its earliest stages of development. In fact, we can sometimes reduce pressure on your feet to prevent an ulcer from forming.
What's the Best Way to Heal a Diabetic Ulcer?
While there are all types of advanced wound dressings, including growth factor therapy and specialized skin substitutes, nothing is as important as controlling the pressure that causes ulcers to form in the first place.
It makes sense if you think about it. The pressure beneath the diabetic foot ulcer is the cause of the problem; the wound is simply the result of that pressure. TAs such, if we want to successfully treat the ulcer, we need to heal the wound while simultaneously controlling the pressure. Unfortunately, this important element of wound care is overlooked by many practitioners and resisted by many patients.
Offloading a wound properly requires some inconvenience and disruption in your lifestyle. Different doctors use different methods to remove the pressure from a wound. Some apply casts, others use a cast boot, and still others use a specialized healing shoe. There are even times where surgery may be needed to remove the pressure from the ulcer site. Adding padding to your existing shoes, or even using diabetic shoes, is not sufficient to keep the pressure away once an ulcer has formed. You must follow all pressure-removal guidelines to ensure proper healing.
Follow-up Care: What to Do After We Heal a Diabetic Ulcer?
After your diabetic foot ulcer is healed, you are not completely out of the woods. It is vital to continue controlling the pressure on your foot, to prevent the wound from returning. This is where a diabetic shoe is appropriate.
Of course, the best way to treat a diabetic foot ulcer is to prevent one from forming. Every person with diabetes should be seen regularly by a podiatrist in Houston to identify and manage risk factors and to ensure that you are wearing the proper shoes. You can also engage in lifestyle habits, such as getting regular, low-impact exercise. Your diet will also play an important role in your on-going recovery. Make sure you get protein at every meal, and take in plenty of vitamins and minerals--these materials will help you repair existing damage and build healthy new tissue. Staying hydrated is also important, as proper hydration helps your blood carry nutrients to your feet more effectively.
If you or someone you love has diabetes, especially if you are concerned about a diabetic foot ulcer forming or not healing, contact Dr. Andrew Schneider for an immediate appointment. With early treatment, we have the tools to achieve healing success rates of close to 95% or higher. Now, the healing timeline varies, depending on the size and the severity of the ulcer at the time when you come in to begin treatment. Typically, however, you can expect small ulcers to heal within four to six weeks, while larger, more complicated ulcers can take twelve to sixteen weeks for complete healing. While that timeline can sound daunting, there's one thing that's clear: the sooner you start the treatment process, the sooner you can expect to achieve complete healing. So don't waste another day wondering what's the best way to heal a diabetic ulcer. Just reach out to our team to request assistance When you call the office, say "I'm diabetic and have a problem" and we'll get you in right away.